When people are reluctant to accept science, or recommendations based on science, my curiosity comes alive. When that person is a twenty years-long friend, I’m even more curious. Matt* is my late husband’s best friend and we talk a lot about topics typically off the table: religion, politics and covid vaccination.
It turns out, seven months into vaccine availability for his risk group, Matt is still not vaccinated. I was vaccinated at my first opportunity. Our chats about covid vaccines have ramped up as his deadline of workplace mandated vaccination looms.
Since I knew these would be ongoing conversations and not just a one-time thing, I wanted to think more about Matt’s background to see if there might be some clues to his perspective. If I were to profile Matt, I’d note that he was raised as an evangelical Christian but no longer practices; graduated college; is a politically moderate gay man; he doesn’t sleep well so has time on his hands; he consumes podcasts, alternative channels and mainstream news more than most people I know; he fact checks sources when he has time; he’s considered going into local politics to be a changemaker; he’s held numerous jobs including realtor, ELL instructor in Taiwan, maintenance supervisor, painter and beer guy at the stadiums.
At first I was just overwhelmed with how much Matt was reading and sharing with me regarding his vaccine hesitancy. Mostly I just listened to him and then started watching and reading the information he referenced. One afternoon at Cowen Park, after our 5th or 6th impromptu talk on covid vaccines, I had this “Dolby sound” moment where things just coalesced.
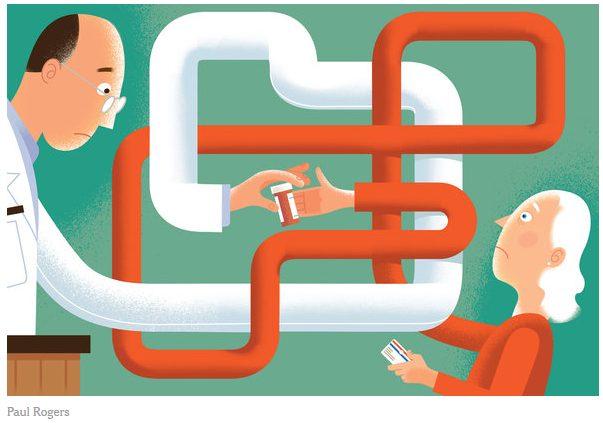
Matt doesn’t trust the pharmaceutical industry. But he never said this directly.
Matt thinks his immune system is capable and doesn’t need priming by a vaccine. But he never said this directly.
According to Dr. Amitabha “Guppy” Gupta, one of Fred Hutch’s philanthropy scientific content analysts, people form mental anchors, or deeply-tethered ways of thinking, about things. In Matt’s case, his main anchor is distrust of the pharmaceutical industry. One of his secondary anchors is the belief that his body’s immune response outperforms influences from pharmaceuticals.
Once I recognized Matt’s anchors (after hours of listening and hours of watching his YouTube suggestions), I realized that all along he sought and presented tons of data to back up his deeply-tethered beliefs. The way Matt seeks data is a kind of confirmation bias, or “myside bias.” Probably unknowingly, Matt seeks information that supports his anchors. Most of us do! To be fair he does sometimes receive information counter to these anchors, especially when I openly disagree with conclusions/experts/data that we’ve discussed.
So I summarized back to Matt: “Tell me if I’m wrong, but it sounds to me like you don’t trust the pharmaceutical companies and you’re worried that the vaccine will mess with your immune system.”
Matt actually looked peaceful. I think just being understood and feeling respected made a big difference for him. Don’t get me wrong. Matt didn’t run out and get the jab because of our talks. But our friendship grew deeper and I feel we can talk about this anytime with mutual respect.
During NWABR’s recent Communication Workshop I was asked how to overcome negative feelings towards people with whom we strongly disagree. Remember that not everyone is a good candidate for a feisty conversation. Discern when to engage and when to let things go. If you let it go, release the conversation with uber-politeness. For example, “I know you’ve put a lot of thought into this. I admire your passion.” If you decide to engage, it’s important to remember that in these dichotomous situations your best bet is to surprise your person with a willingness to compassionately listen to their perspective; this is not about winning an argument. Secondly, see your person as a human being. As someone’s child. When I do this I see my person with love and respect along with a desire to care and lift them up. Remember that their view on covid vaccines isn’t what defines them or their character.
Walking with someone as you disagree with them is not easy, but from personal experience I highly recommend the journey. Best wishes on yours.
*I’ve shared these stories with Matt’s permission.
Jen Wroblewski, MPH, is Public Engagement Manager at Northwest Association for Biomedical Research (NWABR). She co-founded Seattle’s Science on Tap and is a public science communication advocate. Jen welcomes your thoughts and questions on this article: engagement@nwabr.org.

 Last month we left off the story of Joshua Frase, his sister Isabella, and their parents Paul and Alison with their determination to find a treatment for a faulty MTM1 gene, which results in the fatal and physically devastating neuromuscular disease, Myotubular Myopathy (MTM).
Last month we left off the story of Joshua Frase, his sister Isabella, and their parents Paul and Alison with their determination to find a treatment for a faulty MTM1 gene, which results in the fatal and physically devastating neuromuscular disease, Myotubular Myopathy (MTM). Facilitated by Kevin Measor, PhD, Gonzaga University, and Jen Wroblewski, MPH, NWABR on April 10, 2018
Facilitated by Kevin Measor, PhD, Gonzaga University, and Jen Wroblewski, MPH, NWABR on April 10, 2018 If you are a parent you already know the guts, fortitude, desire and village it takes to raise a child from milestone to milestone to adulthood. Imagine your child is born with a fatal genetic disease affecting the function of all his skeletal muscles. Meet Alison and Paul Frase, their daughter Isabella, and finally their son Joshua who was born with myotubular myopathy. If you remember anything about their story, I want you to remember the power of passionate parents working with brilliant, dedicated scientists who tenaciously act and hope for a cure through biomedical research.
If you are a parent you already know the guts, fortitude, desire and village it takes to raise a child from milestone to milestone to adulthood. Imagine your child is born with a fatal genetic disease affecting the function of all his skeletal muscles. Meet Alison and Paul Frase, their daughter Isabella, and finally their son Joshua who was born with myotubular myopathy. If you remember anything about their story, I want you to remember the power of passionate parents working with brilliant, dedicated scientists who tenaciously act and hope for a cure through biomedical research. voted three times on the matter and all times chosen not to introduce fluoride to the drinking water. The most recent vote in 2000 failed by 1%.
voted three times on the matter and all times chosen not to introduce fluoride to the drinking water. The most recent vote in 2000 failed by 1%.